Multiple Requests with Same PAR Type in One Submission
For all PAR types other than Medication, if the health care provider submits multiple request items of the same PAR type on a PAR, these requests will be processed as a group under one PAR ID.
Reviewers will follow the same processes outlined in the Level 1 and Level 2 instructions for responding to a PAR, however, a final determination for the PAR is not reached until all the requests on the PAR have been determined as final.
For example, if there are two DME requests submitted on a PAR and one DME request is granted and the other DME request is denied for medical reasons at the insurer Level 1 review, both requests will move to the insurer Level 2 review. The Level 2 reviewer will issue a decision on both items. The Level 2 reviewer also grants one item and denies the other item. The PAR Status on the My PARs tab will show L-2 Denied. If the health care provider chooses to escalate, the denial to Level 3 review by the Board's Medical Director's Office, they may proceed with the PAR items that were granted, however the PAR won't be moved to the Prior Auth > Resolved tab, until the MDO makes a determination on the escalated item(s).
Responding to Multiple Requests
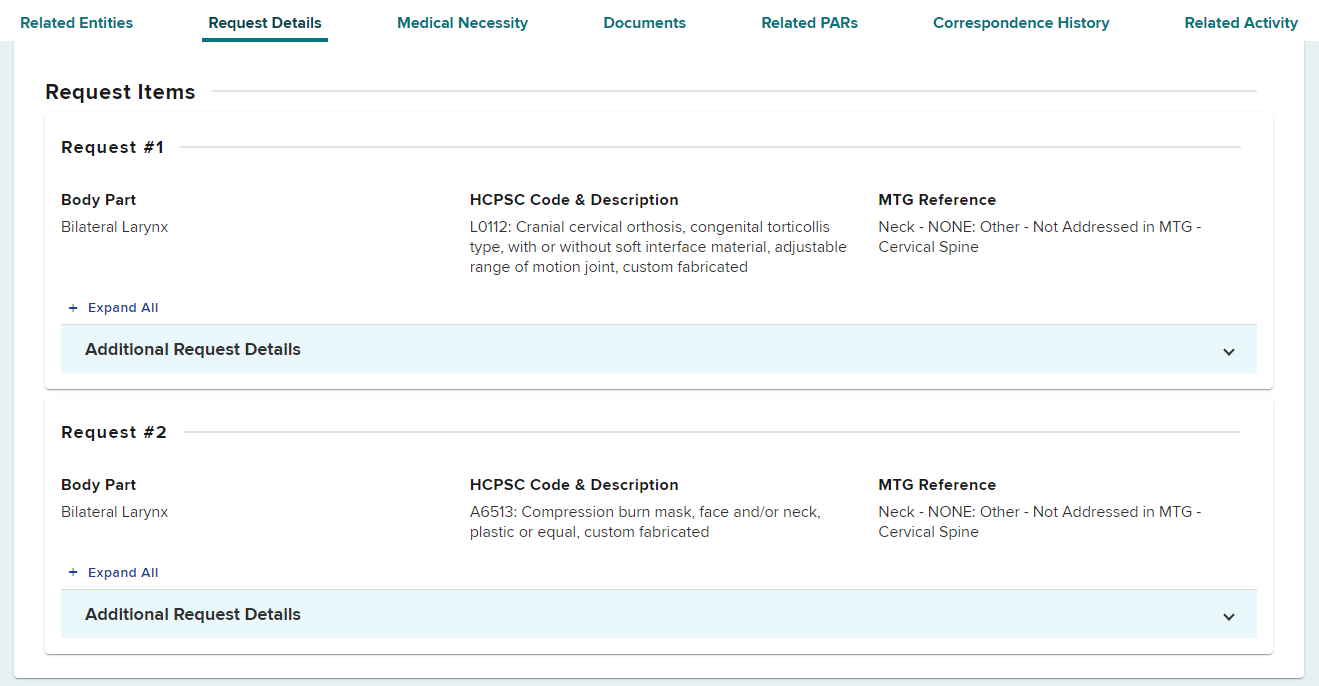
After selecting the PAR ID link in your dashboard, the request details of the PAR details page will show numerous requests.
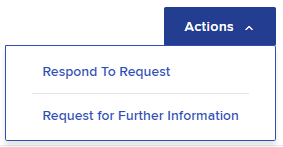
Select Actions and Respond to Request.
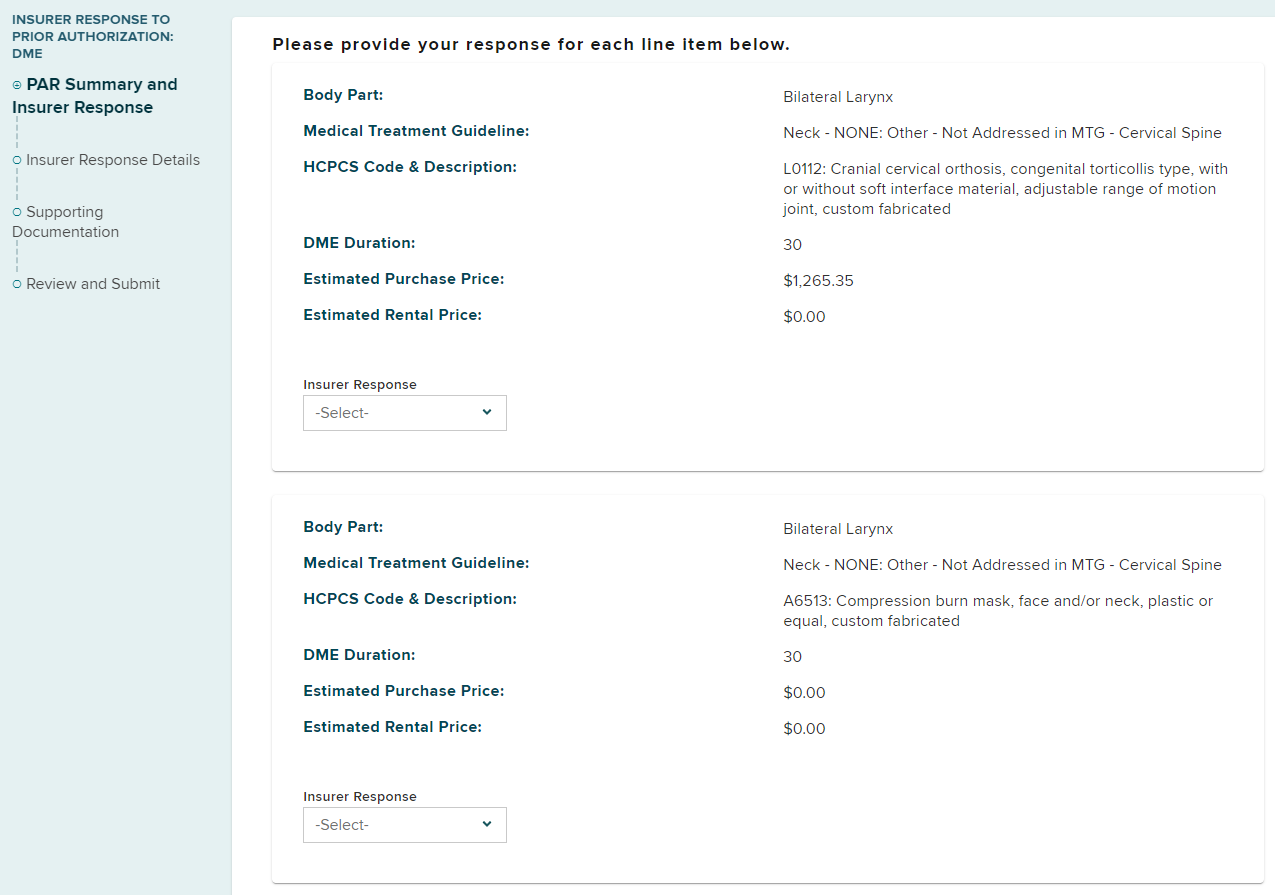
Select the insurer response for each requested item.
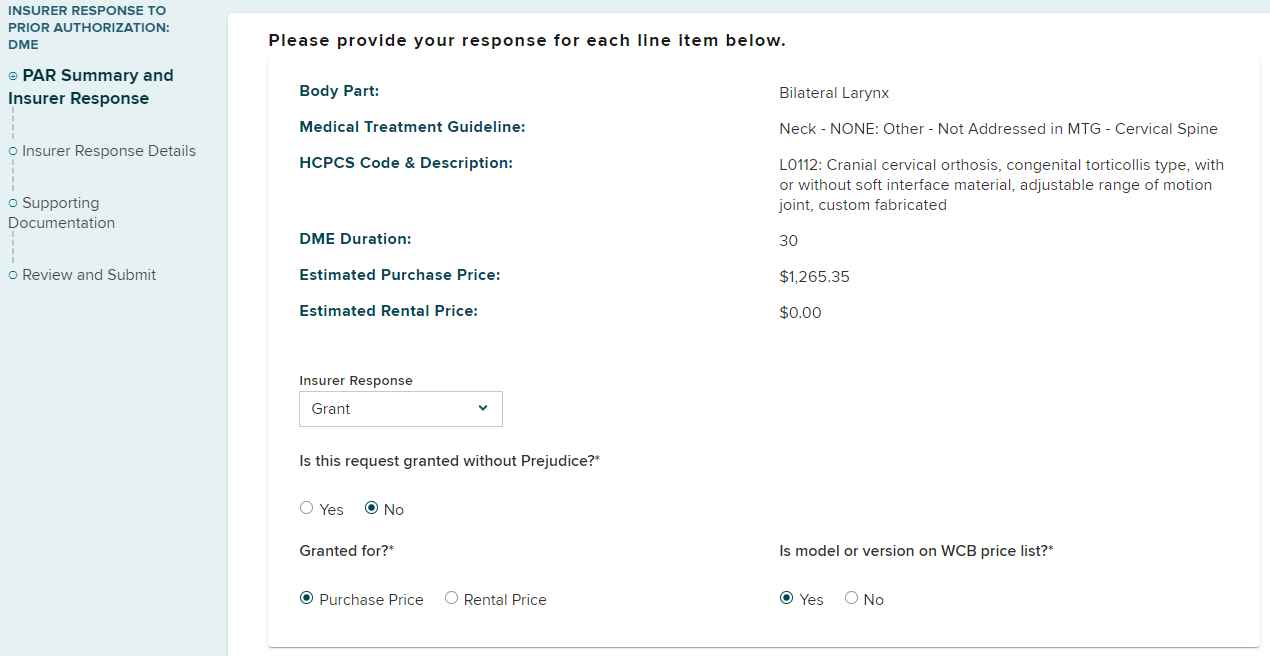
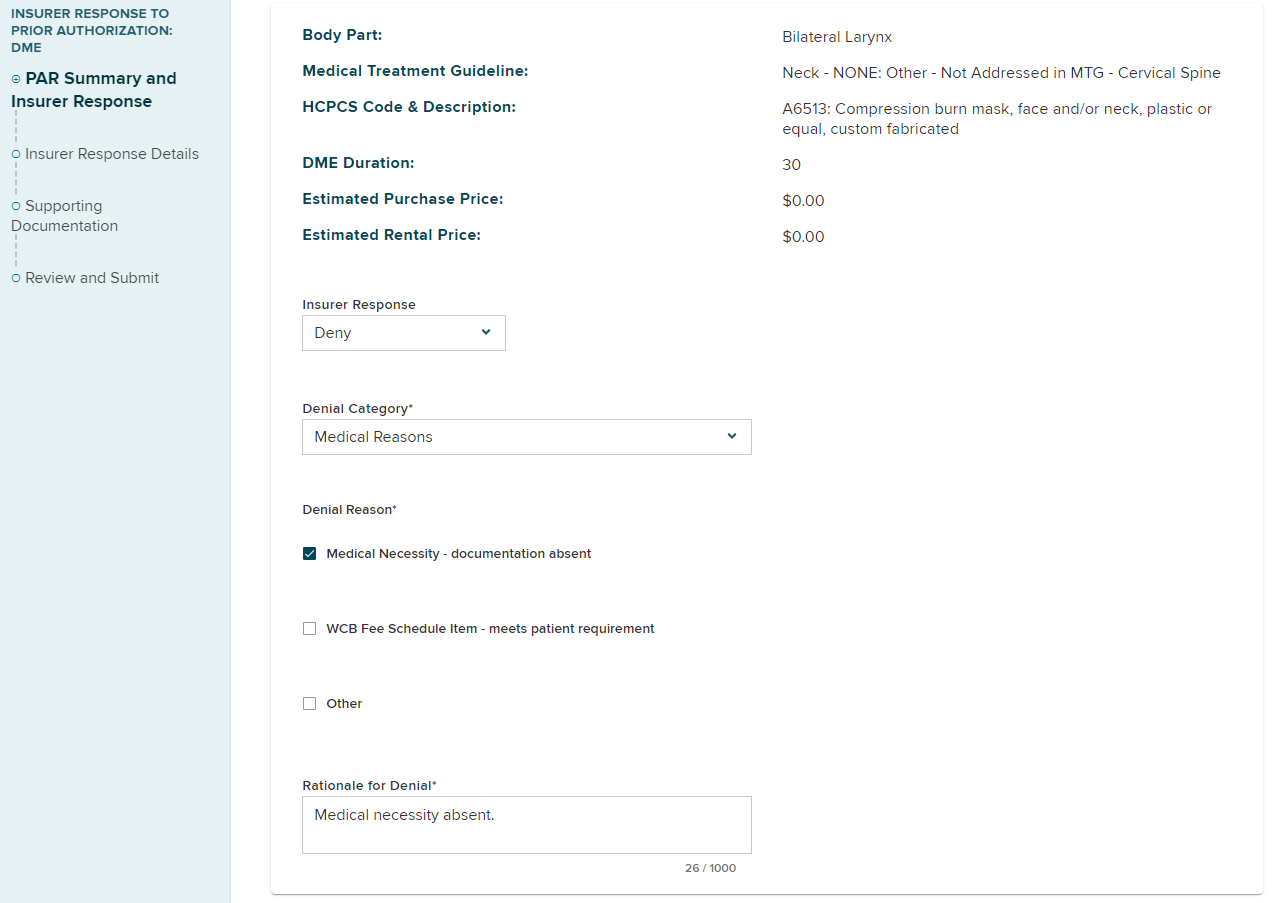
The below example shows that request #1 is granted, while request #2 is denied.
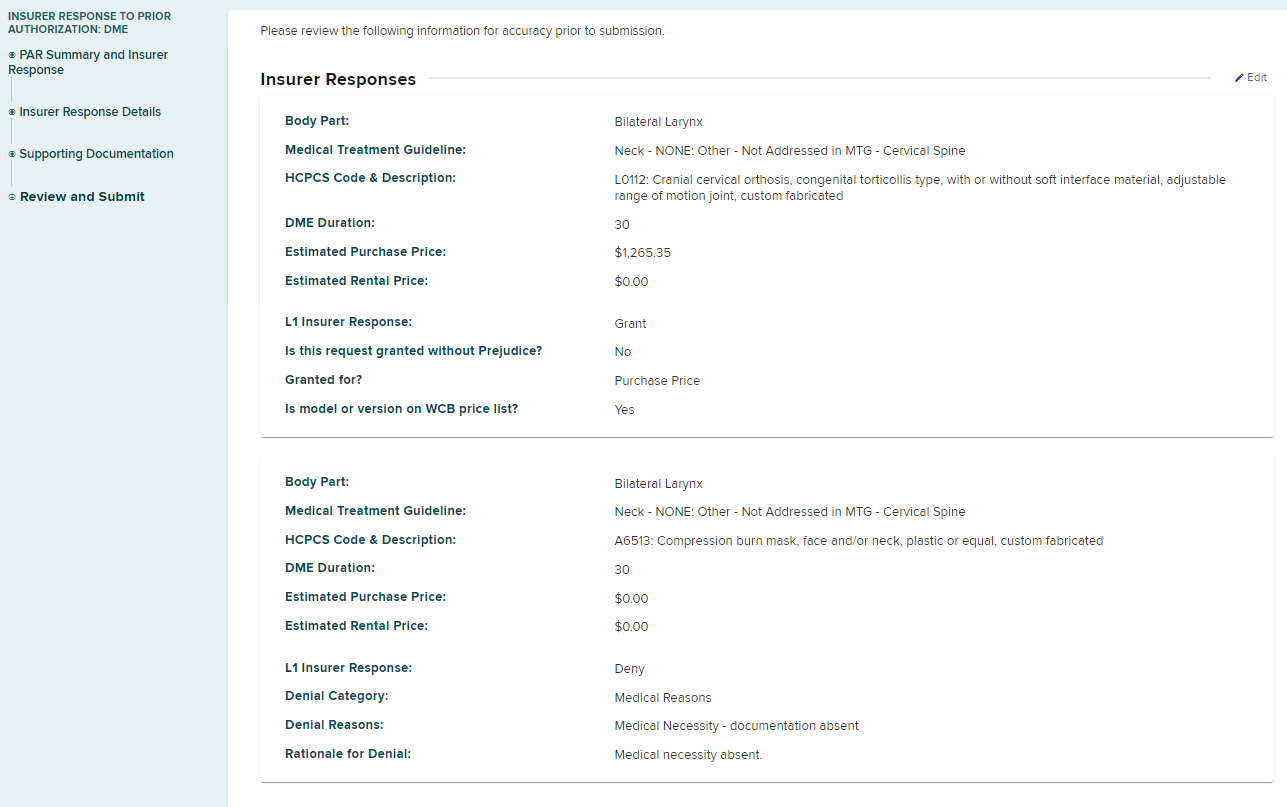
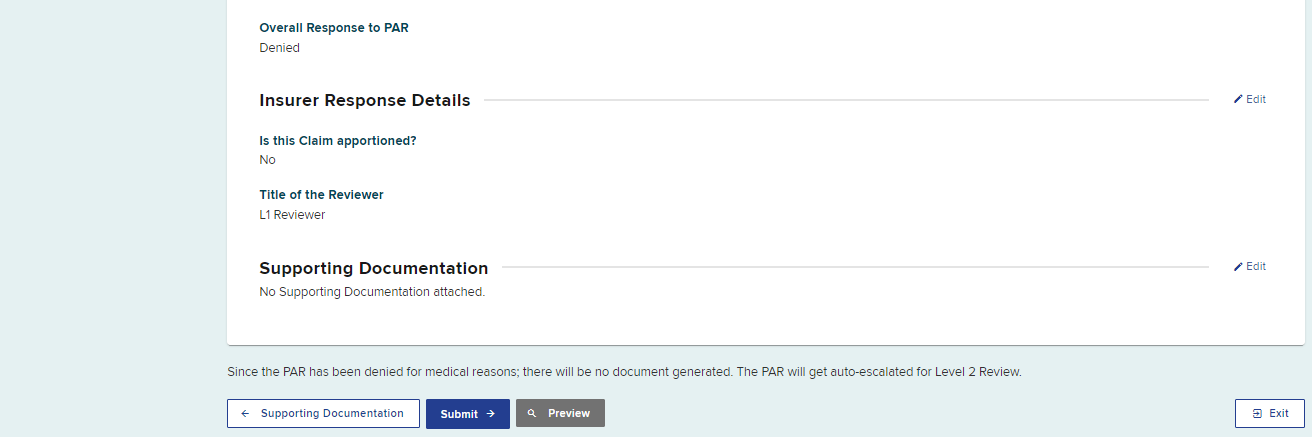
The confirmation screen will show an overall response to the DME PAR is a denial, due to request #2 being denied.
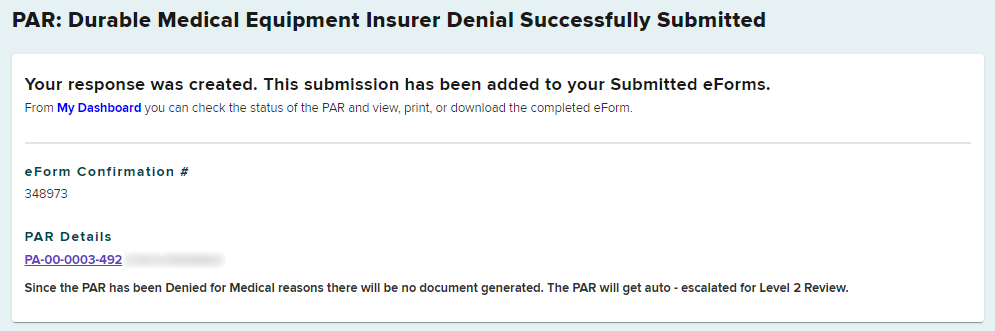
In the Submitted eForms tab, the eForm Name will show as a denial. Select the eForm Details PAR ID link to view details of your submission.
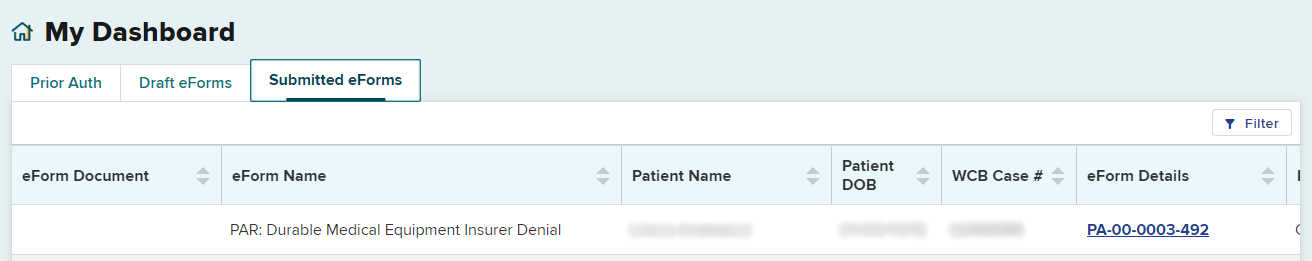
This DME PAR example will continue to Level 2 review because the denial is for a medical reason. The Level 2 reviewer will provide a response to both DME requests, even though one of the items was granted by the Level 1 reviewer. When all requests in the single PAR submission receive a final determination, the PAR submission will move to the Resolved tab.
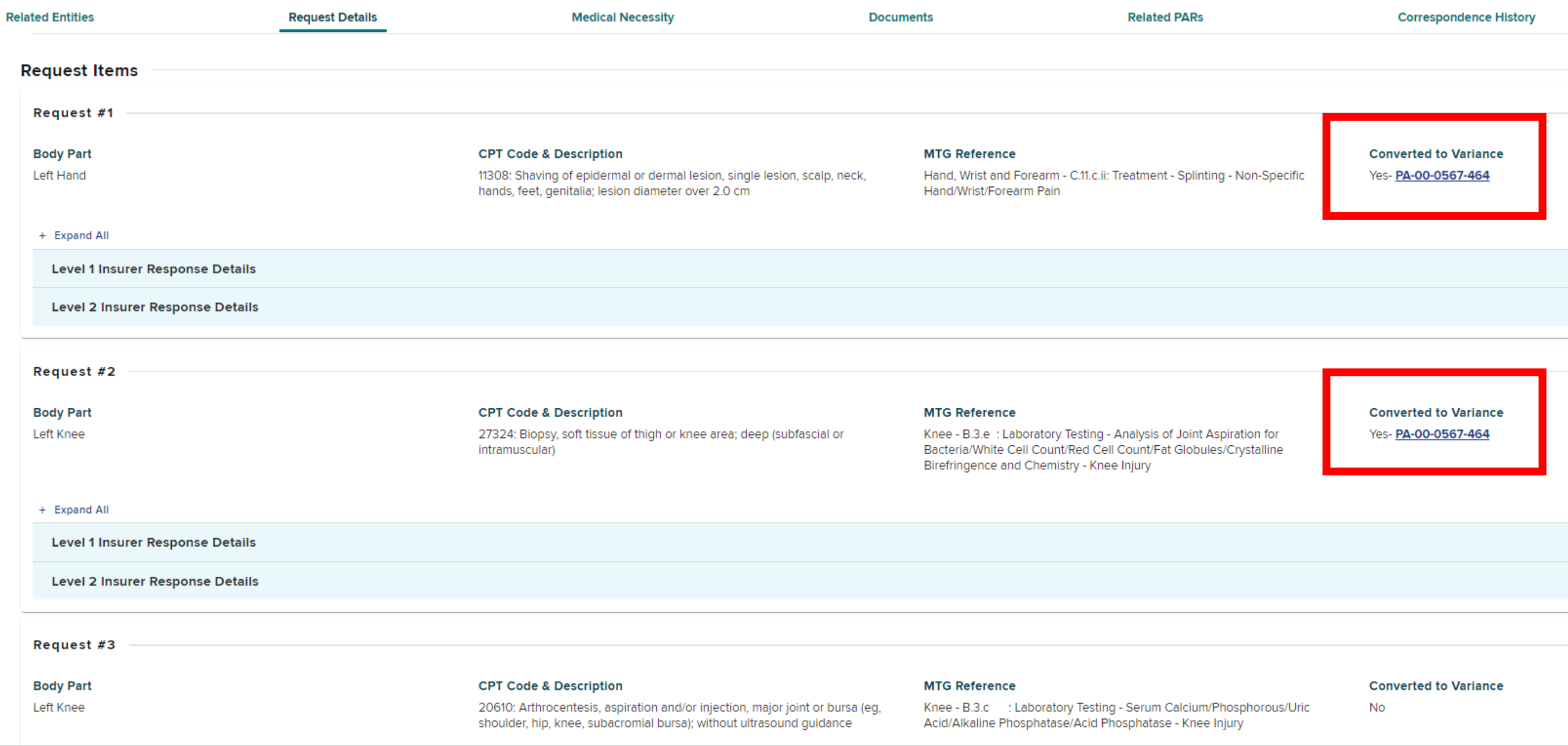
If a prior authorization request contains multiple request items and a provider has converted one or more MTG Confirmations to MTG Variances, those request items will show "Converted to Variance" as Yes and contain a link to the Variance request.